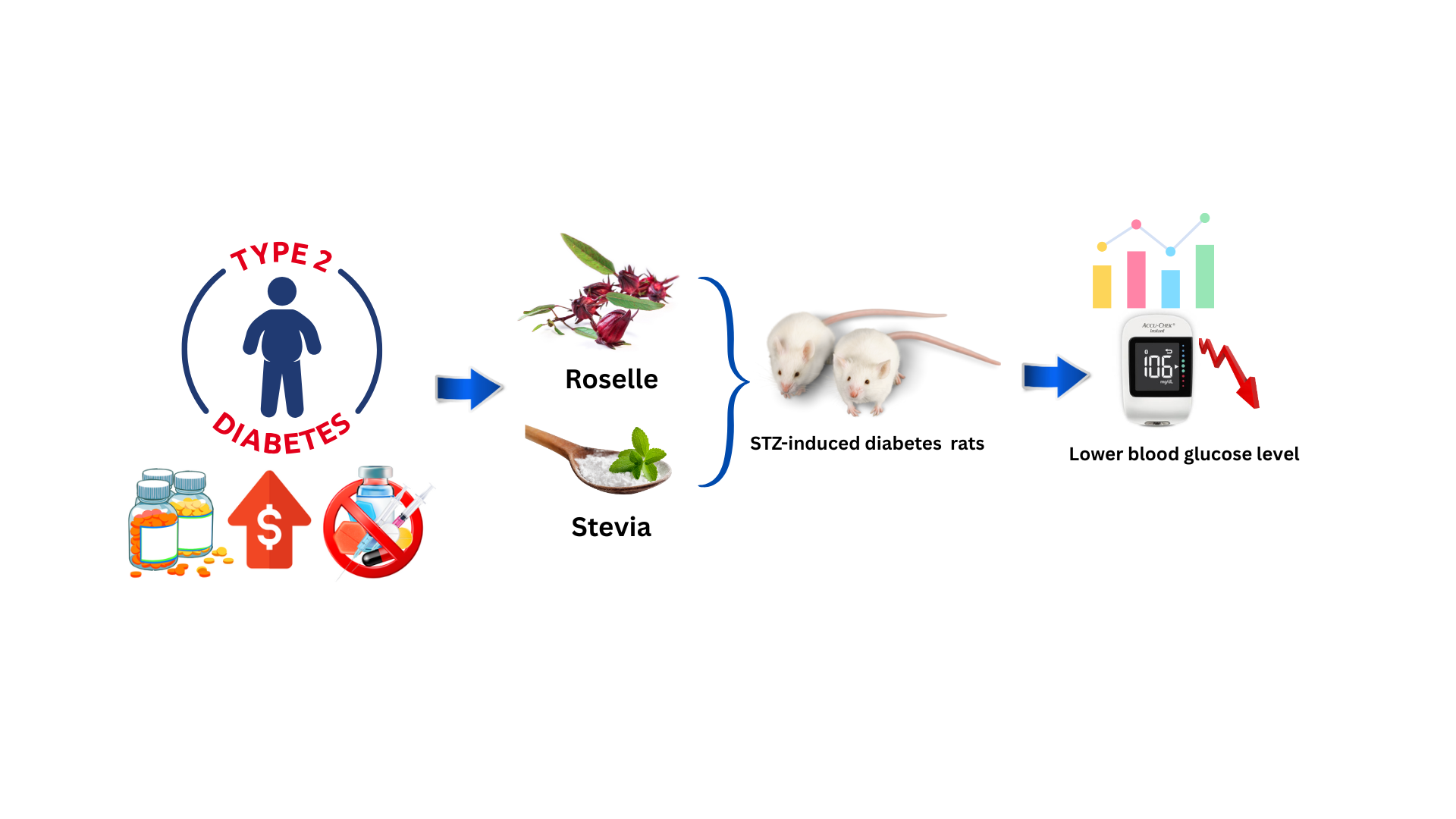
Antidiabetic activity of combined extracts of Hibiscus sabdariffa Linn. and Stevia rebaudiana Bert. on streptozotocin-induced diabetes Wistar rats
DOI:
https://doi.org/10.22437/chp.v9i2.46449Kata Kunci:
blood glucose level, extract, herbal, medicinal plants, post-prandial glucoseAbstrak
The increasing prevalence of diabetes mellitus and the limitation in its conventional therapies underscores the need for alternative treatments. Hibiscus sabdariffa Linn. and Stevia rebaudiana Bert. have demonstrated individual antidiabetic activities attributed to their secondary metabolites, including flavonoid and phenolic compounds. This study employed an experimental in vivo design using rats induced with STZ. Thirty rats were divided into five groups (n=6): normal control, negative control, positive control (Glibenclamide), and two treatment groups receiving the combined aqueous extracts of H.sabdariffa and S.rebaudiana (RSAE) at 500 and 1000 mg/kgBW. Diabetes was induced using STZ (50 mg/kgBW administered i.p). Blood glucose levels were measured fasting and 2 hr postprandial at days 0, 3, and 14 after administration of RSAE. Data were analyzed using One-Way ANOVA. RSAE exhibited dose‐dependent hypoglycaemic activity in STZ‐induced diabetic rats, significantly reducing (p < .005) fasting blood glucose by up to 50.7 % and two‐hour post‐prandial glucose by 44.97% at 1000 mg/kgBW.
Unduhan
Referensi
[1]. International Diabetes Federation IDF Diabetes Atlas, 11th Edn.; Brussels, Belgium, 2025;
[2]. Feingold K Oral and Injectable (Non-Insulin) Pharmacological Agents for the Treatment of Type 2 Diabetes. In Endotext; Feingold KR, Ahmed SF, Anawalt B, Eds.; 2024.
[3]. Richardson,C.R., Borgeson, J.R., Van Harrison R Management of Type 2 Diabetes Mellitus. In Ann Arbor (MI): Michigan Medicine; University of Michigan, 2021.
[4]. Sahin, I.; Bakiner, O.; Demir, T.; Sari, R.; Atmaca, A. Current Position of Gliclazide and Sulfonylureas in the Contemporary Treatment Paradigm for Type 2 Diabetes: A Scoping Review. Diabetes Therapy 2024, 15, 1687–1716, https://doi.org/10.1007/s13300-024-01612-8.
[5]. Padhi, S., Nayak, A.K., Behera, A. Type II Diabetes Mellitus: A Review on Recent Drug Based Therapeutics. Biomedicine & Pharmacotherapy, 2020, 131, 110708, https://doi.org/10.1016/j.biopha.2020.110708.
[6]. Ling, Z., Wang, Q., Stangé, G., In’t Veld, P., Pipeleers, D. Glibenclamide Treatment Recruits Beta-Cell Subpopulation into Elevated and Sustained Basal Insulin Synthetic Activity. Diabetes, 2006, 55, 78–85.
[7]. Jacob, B.; Narendhirakannan, R.T. Role of Medicinal Plants in the Management of Diabetes Mellitus: A Review. 3 Biotech 2018, 9, 4, https://doi.org/10.1007/s13205-018-1528-0.
[8]. Yedjou, C.G.; Grigsby, J.; Mbemi, A.; Nelson, D.; Mildort, B.; Latinwo, L.; Tchounwou, P.B. The Management of Diabetes Mellitus Using Medicinal Plants and Vitamins. International journal of molecular sciences, 2023, 24(1).https://doi.org/10.3390/ijms24109085.
[9]. Amos, A.; Khiatah, B. Mechanisms of Action of Nutritionally Rich Hibiscus Sabdariffa’s Therapeutic Uses in Major Common Chronic Diseases: A Literature Review. Journal of the American Nutrition Association, 2022, 41, 116–124, https://doi.org/10.1080/07315724.2020.1848662.
[10]. Bule, M.; Albelbeisi, A.H.; Nikfar, S.; Amini, M.; Abdollahi, M. The Antidiabetic and Antilipidemic Effects of Hibiscus Sabdariffa: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Food Research International, 2020, 130, https://doi.org/10.1016/j.foodres.2020.108980.
[11]. Mozaffari-Khosravi, H.; Jalali-Khanabadi, B.-A.; Afkhami-Ardekani, M.; Fatehi, F.; Noori-Shadkam, M. The Effects of Sour Tea (Hibiscus Sabdariffa) on Hypertension in Patients with Type II Diabetes. J Hum Hypertens 2009, 23, 48–54, https://doi.org/10.1038/jhh.2008.100.
[12]. 12. Salem, M.A.; Zayed, A.; Beshay, M.E.; Abdel Mesih, M.M.; Ben Khayal, R.F.; George, F.A.; Ezzat, S.M. Hibiscus Sabdariffa L.: Phytoconstituents, Nutritive, and Pharmacological Applications. Advances in Traditional Medicine 2022, 22, 497–507, https://doi.org/10.1007/s13596-020-00542-7.
[13]. Adeyemi, D.O.; Adewole, O.S. Hibiscus Sabdariffa Reduces Renal Damage in Experimental Streptozotocin-Induced Diabetes. Journal of Morphological Sciences, 2020, 37, 2–12, https://doi.org/10.51929/jms.37.2.2020.
[14]. Haro, G. Antidiabetic Effect of Roselle Calyces Extract (Hibiscus sabdariffa L.) in Streptozotocin Induced Mice. International Journal of PharmTech Research, 2014, 6(5), 1703–1711.
[15]. Salleh, N.H.; Zulkipli, I.N.; Mohd Yasin, H.; Ja’Afar, F.; Ahmad, N.; Wan Ahmad, W.A.N.; Ahmad, S.R. Systematic Review of Medicinal Plants Used for Treatment of Diabetes in Human Clinical Trials: An ASEAN Perspective. Evidence-based Complementary and Alternative Medicine 2021, https://doi.org/10.1155/2021/5570939
[16]. Susilawati, Y.; Febriyanti, R.M.; Febrina, E.; Chaerunisaa, A.; Sumiwi, S.A. A Comprehensive in Vivo Study of the Antihypertensive Properties and Toxicity of Roselle (Hibiscus sabdariffa L.). Pharmacia 12AD, 70, 1521–1530. https://doi.org/10.3897/pharmacia.70.e109119.
[17]. Amin, A.R.; Kassab, R.B.; Abdel Moneim, A.E.; Amin, H.K. Comparison Among Garlic, Berberine, Resveratrol, Hibiscus Sabdariffa, Genus Zizyphus, Hesperidin, Red Beetroot, Catha Edulis, Portulaca Oleracea, and Mulberry Leaves in the Treatment of Hypertension and Type 2 DM: A Comprehensive Review. Nat Prod Commun 2020, 15, https://doi.org/10.1177/1934578X20921623.
[18]. Mojica, L.; Rui, L.; Gonzalez De Mejia, E. Hibiscus sabdariffa L. Phytochemical Composition and Nutraceutical Properties. ACS Symposium Series 2012, 1109, 289–305, doi:10.1021/bk-2012-1109.ch017.
[19]. Abdullah, B.; Khairunnisa, S.D.; Muhammad, M.I.; Atwinda, R.S. Isolation of Anthocyanin from Indonesian Purple Roselle (Hibiscus sabdariffa L.) Calyces. In Proceedings of the AIP Conference Proceedings; 2020; 2197.
[20]. Alegbe, E.O.; Teralı, K.; Olofinsan, K.A.; Surgun, S.; Ogbaga, C.C.; Ajiboye, T.O. Antidiabetic Activity-Guided Isolation of Gallic and Protocatechuic Acids from Hibiscus Sabdariffa Calyxes. J Food Biochem, 2019, 43, https://doi.org/10.1111/jfbc.12927.
[21]. Anjabtsawa, D.; Febriyanti, R.M.; Diantini, A. Exploring the Phytochemical Properties and Therapeutic Potential of Hibiscus Sabdariffa Linn. and Stevia Rebaudiana Bert. Indonesian Journal of Biological Pharmacy, 2025, 4(2), 91-102. https://doi.org/10.24198/ijbp.v4i2.54035.g24888
[22]. Ajiboye, B.O.; Famusiwa, C.D.; Ajaesowuonu, J.F.; Chibueze, O.P.; Adejumo, A.A.; Onikanni, S.A.; Ajeigbe, K.O.; Ajuwon, O.R.; Oyinloye, B.E. Flavonoid-Rich Extracts of Hibiscus Sabdariffa Leaf Attenuate Cardiomyopathy in Streptozotocin-Induced Rats. Comp Clin Path 2024, 33, 927–941, https://doi.org/10.1007/s00580-024-03615-0.
[23]. Khilar, S.; Singh, A.P.; Biagi, M.; Sharma, A. An Insight into Attributes of Stevia rebaudiana Bertoni: Recent Advances in Extraction Techniques, Phytochemistry, Food Applications and Health Benefits. Journal of Agriculture and Food Research, 2022, 10, 100458, https://doi.org/10.1016/j.jafr.2022.100458.
[24]. Peteliuk, V.; Rybchuk, L.; Bayliak, M.; Storey, K.B.; Lushchak, O. Natural Sweetener Stevia Rebaudiana: Functionalities, Health Benefits and Potential Risks. EXCLI Journal, 20, 1412–1430. https://doi.org/10.17179/excli2021-4211
[25]. Kamal, N.H.; Essmat, A.; El Askary, H.I.; El Hefnawy, H.M.; Wahab, S.M.A.; Meselhy, M.R. Chemical Profile and Beneficial Effect of Standardized Extract of Stevia Rebaudiana Bertoni Leaves on Metabolic Syndrome in High Fat Diet Streptozotocin-Induced Diabetic Rats. Applied Biological Chemistry, 2022, 65(5), https://doi.org/10.1186/s13765-022-00724-8.
[26]. Patel, S.; Navale, A. The Natural Sweetener Stevia: An Updated Review on Its Phytochemistry, Health Benefits, and Anti-Diabetic Study. Current diabetes reviews, 20(2), https://doi.org/10.2174/1573399819666230501210803
[27]. Shahu, R.; Jobby, R.; Patil, S.; Bhori, M.; Tungare, K.; Jha, P. Phytochemical Content and Antioxidant Activity of Different Varieties of Stevia rebaudiana. Horticulture, Environment, and Biotechnology, 2022, 63, 935–948, https://doi.org/10.1007/s13580-022-00451-5.
[28]. Febriyanti, R.M.; Putri, R.N.; Diantini, A.; Levita, J. Hypoglycaemic Properties of The Combination of Roselle Calyx (Hibiscus sabdariffa Linn.) and Stevia Leaves (Stevia rebaudiana B.) in Alloxan-Induced White Rats. Indonesian Journal of Pharmaceutical Science and Technology 2025, 12, 90–97, https://doi.org/10.24198/ijpst.v12s2.59646.
[29]. Anjabtsawa, D.; Febriyanti, R.M.; Diantini, A. A Review of Antidiabetic Potential of Indonesian Medicinal Plants on Streptozotocin (STZ)-Induced Rats. Indonesian Journal of Biological Pharmacy, 2024, 4(1), 24–37. https://doi.org/10.24198/ijbp.v4i1.54037
[30]. Radenković, M.; Stojanović, M.; Prostran, M. Experimental Diabetes Induced by Alloxan and Streptozotocin: The Current State of the Art. J Pharmacol Toxicol Methods 2016, 78, 13–31, https://doi.org/10.1016/j.vascn.2015.11.004.
[31]. Singh, R.; Gholipourmalekabadi, M.; Shafikhani, S.H. Animal Models for Type 1 and Type 2 Diabetes: Advantages and Limitations. Front Endocrinol (Lausanne) 2024, 15, 1359685, https://doi.org/10.3389/fendo.2024.1359685.
[32]. Pandey, S.; Chmelir, T.; Chottova Dvorakova, M. Animal Models in Diabetic Research—History, Presence, and Future Perspectives. 11(10), 2852. https://doi.org/10.3390/biomedicines11102852
[33]. Ghasemi, A.; Jeddi, S. Streptozotocin as a Tool for Induction of Rat Models of Diabetes: A Practical Guide. EXCLI J 2023, 22, 274–294, https://doi.org/10.17179/excli2022-5720.
[34]. Deeds, M.C; Anderson, J.M., Armstrong, A.S., Gastineau, D.A., Hiddinga, H.J. Jahangir, A., Eberhardt, N.L., Kudva, Y.C., Single Dose Streptozotocin-Induced Diabetes: Considerations for Study Design in Islet Transplantation Models. Laboratory animals, 2011, 45(3), 131–140. https://doi.org/10.1258/la.2010.010090
[35]. Galindo, R.J.; Trujillo, J.M.; Low Wang, C.C.; McCoy, R.G. Advances in the Management of Type 2 Diabetes in Adults. BMJ Medicine 2023, 2, e000372, https://doi.org/10.1136/bmjmed-2022-000372.
[36]. Rizza, R.A. Pathogenesis of Fasting and Postprandial Hyperglycemia in Type 2 Diabetes: Implications for Therapy. Diabetes 2010, 59, 2697–2707, https://doi.org/10.2337/db10-1032.
[37]. Lu, X.; Xie, Q.; Pan, X.; Zhang, R.; Zhang, X.; Peng, G.; Zhang, Y.; Shen, S.; Tong, N. Type 2 Diabetes Mellitus in Adults: Pathogenesis, Prevention and Therapy. Signal Transduct Target Ther 2024, 9, 262, https://doi.org/10.1038/s41392-024-01951-9.
[38]. Su, Q.; Liu, J.; Li, P.; Qian, L.; Yang, W. Relative Contribution of Fasting and Postprandial Blood Glucose in Overall Glycemic Control: Post Hoc Analysis of a Phase IV Randomized Trial. Diabetes Ther 2018, 9, 987–999, https://doi.org/10.1007/s13300-018-0403-7.
[39]. Ketema, E.B.; Kibret, K.T. Correlation of Fasting and Postprandial Plasma Glucose with HbA1c in Assessing Glycemic Control; Systematic Review and Meta-Analysis. Arch Public Health 2015, 73, 43, https://doi.org/10.1186/s13690-015-0088-6.
[40]. Ifie, I., Marshall, L.J., Ho, P., Williamson, G. Hibiscus sabdariffa (Roselle) Extracts and Wine: Phytochemical Profile, Physicochemical Properties, and Carbohydrase Inhibition. Journal of agricultural and food chemistry, 2016, 64, 4921–4931, https://doi.org/10.1021/acs.jafc.6b01246.
[41]. Jamrozik, D.; Borymska, W.; Kaczmarczyk-Żebrowska, I. Hibiscus Sabdariffa in Diabetes Prevention and Treatment—Does It Work? An Evidence-Based Review. Foods 2022, 11, https://doi.org/10.3390/foods11142134.
[42]. Joseph, D.; George, J.; Mathews, M.M.; Mathew, F.; Varghese, B.; Sunny, B. A Comprehensive Exploration on Therapeutic Options of Stevia Rebaudiana with Emphasize on Anti-Diabetic Attribute. Research Journal of Pharmacy and Technology, 2019, 12, 4981–4988, https://doi.org/10.5958/0974-360X.2019.00863.1.
[43]. Tong, Y.; Liu, F.; Huang, K.; Li, J.; Yang, X.; Chen, J.; Liu, X.; Cao, J.; Chen, S.; Yu, L.; et al. Changes in Fasting Blood Glucose Status and Incidence of Cardiovascular Disease: The China-PAR project. Journal of diabetes, 15(2), 110–120. https://doi.org/10.1111/1753-0407.13350
[44]. Thiab, S.; Akhal, T.; Akeblersane, M.; Sheth, H.; Atkin, S.L.; Butler, A.E. Microvascular Complications in Prediabetes: A Systematic Review & Meta-Analysis. Diabetes Res Clin Pract 2025, 225, 112261, https://doi.org/10.1016/j.diabres.2025.112261.
[45]. Hershon, K.S.; Hirsch, B.R.; Odugbesan, O. Importance of Postprandial Glucose in Relation to A1C and Cardiovascular Disease. Clinical Diabetes 2019, 37, 250–259, https://doi.org/10.2337/cd18-0040.
[46]. Liu, M.; Liu, C.; Zhaxi, P.; Kou, X.; Liu, Y.; Xue, Z. Research Progress on Hypoglycemic Effects and Molecular Mechanisms of Flavonoids: A Review. Antioxidants 2025, 14, 378, https://doi.org/10.3390/antiox1404037.
[47]. Praparatana, R.; Maliyam, P.; Barrows, L.R.; Puttarak, P. Flavonoids and Phenols, the Potential Anti-Diabetic Compounds from Bauhinia Strychnifolia Craib. Stem. Molecules 2022, 27, 2393, https://doi.org/10.3390/molecules27082393.
[48]. Dimitriadis, G.D.; Maratou, E.; Kountouri, A.; Board, M.; Lambadiari, V. Regulation of Postabsorptive and Postprandial Glucose Metabolism by Insulin-Dependent and Insulin-Independent Mechanisms: An Integrative Approach. Nutrients 2021, 13, 159, https://doi.org/10.3390/nu13010159.
[49]. Kazeem, M.I.; Adamson, J.O.; Ogunwande, I.A. Modes of Inhibition of α -Amylase and α -Glucosidase by Aqueous Extract of Morinda Lucida Benth Leaf. BioMed Research International, 2013, 1–6, https://doi.org/10.1155/2013/527570.
[50]. 50. DU, C.T.; FRANCIS, F.J. Anthocyanins of Roselle (Hibiscus sabdariffa, L.). Journal Food Sciences, 1973, 38, 810–812, https://doi.org/10.1111/j.1365-2621.1973.tb02081.x.
[51]. 51. Lazalde-Cruz, R.; Miranda-Romero, L.A.; Tirado-González, D.N.; Carrillo-Díaz, M.I.; Medina-Cuéllar, S.E.; Mendoza-Martínez, G.D.; Lara-Bueno, A.; Tirado-Estrada, G.; Salem, A.Z.M. Potential Effects of Delphinidin-3-O-Sambubioside and Cyanidin-3-O-Sambubioside of Hibiscus Sabdariffa L. on Ruminant Meat and Milk Quality. Animals 2021, 11, 2827, https://doi.org/10.3390/ani11102827.
[52]. Ademiluyi, A.O.; Oboh, G. Aqueous Extracts of Roselle ( Hibiscus Sabdariffa Linn.) Varieties Inhibit α -Amylase and α -Glucosidase Activities In Vitro. J Med Food 2013, 16, 88–93, https://doi.org/10.1089/jmf.2012.0004
[53]. Feng, S.-Y.; Wu, S.-J.; Chang, Y.-C.; Ng, L.-T.; Chang, S.-J. Stimulation of GLUT4 Glucose Uptake by Anthocyanin-Rich Extract from Black Rice (Oryza sativa L.) via PI3K/Akt and AMPK/P38 MAPK Signaling in C2C12 Cells. Metabolites 2022, 12, 856, https://doi.org/10.3390/metabo12090856.
[54]. Zhang, S.; Gai, Z.; Gui, T.; Chen, J.; Chen, Q.; Li, Y. Antioxidant Effects of Protocatechuic Acid and Protocatechuic Aldehyde: Old Wine in a New Bottle. Evidence-Based Complementary and Alternative Medicine 2021, 2021, 1–19, https://doi.org/10.1155/2021/6139308
[55]. Simlat, M.; Ptak, A.; Wójtowicz, T.; Szewczyk, A. The Content of Phenolic Compounds in Stevia rebaudiana (Bertoni) Plants Derived from Melatonin and NaCl Treated Seeds. Plants 2023, 12, 780, https://doi.org/10.3390/plants12040780.
[56]. Carrera-Lanestosa, A.; Coral-Martínez, T.; Ruíz-Ciau, D.; Moguel-Ordoñez, Y.; Segura-Campos, M.R. Phenolic Compounds and Major Steviol Glucosides by HPLC-DAD-RP and Invitro Evaluation of the Biological Activity of Aqueous and Ethanolic Extracts of Leaves and Stems: S. rebaudiana Bertoni (Creole Variety INIFAP C01). Int J Food Prop 2020, 23, 199–212, https://doi.org/10.1080/10942912.2020.1716789.
[57]. Philippaert, K.; Pironet, A.; Mesuere, M.; Sones, W.; Vermeiren, L.; Kerselaers, S.; Pinto, S.; Segal, A.; Antoine, N.; Gysemans, C.; et al. Steviol Glycosides Enhance Pancreatic Beta-Cell Function and Taste Sensation by Potentiation of TRPM5 Channel Activity. Nat Commun 2017, 8, 14733, https://doi.org/10.1038/ncomms14733
[58]. Ajiboye, B.O.; Famusiwa, C.D.; Falode, J.A.; Okwukwe Akojuru, D.; Owolabi, B.T.; Adejumo, A.A.; Oyinloye, B.E.; Ajuwon, O.R.; Ogedengbe, O.O.; Ojo, O.A. Protective Effects of Flavonoid-Rich Extracts from Hibiscus sabdariffa Leaves on Streptozotocin-Induced Testicular Damage in Rats. Phytomedicine Plus, 2025, 5, 100808, https://doi.org/10.1016/j.phyplu.2025.100808